Global prevalence and distribution of cardiovascular diseases
Cardiovascular diseases (CVD) refers to a diverse range of conditions that affect the heart or blood vessels. Major types of CVDs’ include coronary heart disease, stroke and heart failure. CVDs’, still remain the major cause of death across all the regions of the world. In 2015, approximately 17.7 million people died across the globe due to CVDs’, which represents 31% of total global deaths (WHO, 2017). The established risk factors associated with CVDs’ are obesity, hypertension, diabetes, high cholesterol and smoking (Laslett et al., 2012).
A global statistics of cardiovascular disease prevalence
Global trends in CVD mortality are obtained from a diverse range of country-specific data from several developed and developing countries. Countries with lowest age-standardized prevalence (<5000 cases per 100,000 individuals) include United States, Australia, Canada, Japan, and Singapore. Countries with highest age-standardized prevalence (>9000 cases per 100,000 individuals) include West Africa, Morocco, Oman, Iraq and a few others.

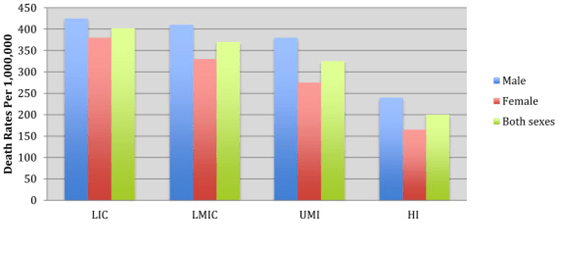
An interesting relationship exists between the social determinant of health and prevalence of Ccardiovascular diseases. In high-income countries such as United States, Australia and northwestern European countries a “rise and fall” pattern of CVD mortality is evident (Bowry et al., 2015). In this pattern, the mortality rate increases, peaks and then declines significantly. On the contrary, low and middle-income countries (LMIC) belonging to East Asia, Latin America and sub-Saharan Africa report a distinct rise pattern in CVD mortality. The WHO indicates that 80% of the total CVD deaths are occurring in LMIC. Interestingly, the deaths arising from the CVDs’ are affecting both males and females equally in the LMIC. This data suggests that due to the growing social and economic burden of health care system, LMIC may not have adequate health infrastructure to handle these pressures.
The figure below shows the occurrence of cardiovascular diseases deaths per 1 million people in different regions; Low Income Countries (LIC), Low and Middle Income Countries (LMIC), Upper Middle Income (UMI) and High Income (HI).
Major countries for cardiovascular diseases
Around 3/4th of the world’s chronic disease related deaths occur from CVD in low-and middle-income countries. This is because, people in these countries do not have the benefit of advanced health care programmes for early detection and treatment of people with risk factors (WHO, 2017).
Eastern sub-Saharan Africa, the Middle East/ North Africa region and South Asia all had similar estimated rates of just over 2,000 prevalent CVD cases per 100,000 populations. More than one-quarter of deaths in sub-Saharan Africa were due to other cardiovascular and circulatory diseases (Roth et al., 2017). Among the higher income nations, Eastern Europe had the highest estimated age-standardized prevalence of Ischemic Heart Disease (IHD) in 2015 (Roth et al., 2017). The figure below represents CVD related deaths’ seasonal patterns among different countries.

Race and ethnicity
With respect to race and ethnicity, the risk of CVD may vary from one place to another. Black adults are at a higher risk of heart diseases than whites. It has been found that black people developed a genetic predisposition to be sensitive to salt, meaning their bodies would retain more salt. This condition allows them to conserve more water, which will be beneficial in hot climates. However, more salt increases the volume of blood, which in turn raises the blood pressure (hypertension) and finally leading to CVD. Similarly, among all the ethnic populations, Indians are the most affected by CVD. The leading factors of CVD between the subgroups of Asians are due to elevated levels of glucose intolerance, central obesity, fasting triglyceride and insulin compared to other populations (Eastwood et al., 2016).
Sex differences
Historically, CVDs’ were perceived as a man’s disease and yet many reports indicate that more women die from CVD each year than men. According to recent WHO reports, overall CVD mortality occurred in 55% of cases in women and 45% cases in men. These gender-based CVD risks are due to differences in pathophysiology, clinical presentation, and management in men and women. Age, hypertension, and cholesterol are the risk factors influencing CVD in men, whereas menopause, diabetes, smoking and triglyceride levels mainly influence women.
The process of diagnosis significantly differs in both sexes, thus making the CVDs’ diagnosis challenging. For example, in myocardial ischemia, typical male symptoms include oppressive chest pain, epigastric pain and shortness of breath. In contrast, for the same condition in women, stinging chest pain, abdominal pain and weakness are the general symptoms. This suggests that CVD symptoms should be estimated based on the gender, irrespective of their pathophysiological mechanisms to improve the prognosis.
Factors affecting cardiovascular diseases globally
Numerous epidemiologic studies have clearly demonstrated the risk factors that are usually associated with CVDs’. These factors can be classified into three types:
- Behavioral risk factors: which are found to strongly influence CVD. These include tobacco, cholesterol and physical inactivity.
- Metabolic risk factors: which increase the chance of developing a CVD. Some examples of these factors are high blood pressure, elevated glucose, and obesity.
- Other factors: which are associated with the CVD but their cause and effect in the progression of CVD remains to be identified.
Some examples of these markers are low socioeconomic status, high prothrombotic factors, and markers of infection.
Major contributors to reduction in cardiovascular diseases mortality
Data from several studies suggest that smoking, blood lipids, and blood pressure are the three most important risk factors for reducing the CVD mortality. Many studies have demonstrated that reduction of these three factors either alone or together reduced the risk of CVD incidence and mortality by up to 50% (Psota et al., 2018). Additionally, changes in the dietary lifestyles also help decline the CVD mortality rate. In addition to these prevention strategies, a significant improvement is visible in evidence-based strategies to reduce CVD deaths. One example is that patients undergoing coronary artery bypass graft surgery reduced the CVD mortality by approximately 10%.
Time to address CVD differently
CVD is a major cause of death and chronic disability around the world with Ischemic Heart Disease and stroke contributing majority to CVD. Taken together, despite the tremendous growth of knowledge and advances in prevention and treatment of CVDs’ the mortality rate still continue to rise. This rise is due to the increasing population and aging as well as increasing prevalence of risk factors. Nonetheless, strategies to address the range of risk factor would certainly prevent the premature deaths associated with CVD.
References
- Bowry, A. D., Lewey, J., Dugani, S. B. & Choudhary, N. K. 2015. The Burden of Cardiovascular Disease in Low- and Middle-Income Countries: Epidemiology and Management. Can J Cardiol, 31, 1151-9.
- Eastwood, S. V., et al. 2016. Ethnic differences in cross-sectional associations between impaired glucose regulation, identified by oral glucose tolerance test or HbA1c values, and cardiovascular disease in a cohort of European and South Asian origin. Diabet Med, 33, 340-7.
- Laslett, L. J., et al. 2012. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J Am Coll Cardiol, 60, S1-49.
- Psota, M., et al. 2018. Explaining the decline in coronary heart disease mortality rates in the Slovak Republic between 1993-2008. PLoS One, 13,
- Roth, G. A., et al. 2015. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation, 132, 1667-78.
- Roth, G. A., Huffman, M. D., Moran, A. E., Feigin, V., Mensah, G. A., Naghavi, M., & Murray, C. J. L. (2015). Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation, 132(17), 1667–78. https://doi.org/10.1161/CIRCULATIONAHA.114.008720
- Stewart, S., Keates, A.K., Redfern, A. and McMurray, J.J., 2017. Seasonal variations in cardiovascular disease. Nature Reviews Cardiology, 14(11), p.654.
- WHO. (2017). Cardiovascular diseases (CVDs). WHO. World Health Organization.
Discuss