Treatment options of lethal Anaphylaxis, allergic Rhinitis & Asthma
The previous articles shed light on the prevalence of allergic diseases across five different geographic locations. Thus showing allergies to be a global problem and exerts considerable socioeconomic burden on the respective nations. Allergic diseases like Anaphylaxis, Rhinitis and Asthma interfere with day to day activities of an individual, resulting in physical and emotional distress. The data on health-related quality of life shows the interference of allergies in work and social life, inhibition of outdoor activities and mobility (Baiardini, Braido, Brandi, & Canonica, 2006), making identification of relevant treatment options important. The present discussion thus aims to highlight the treatment options available for most prevalent allergic disorders.
Anaphylaxis can be lethal
Anaphylaxis is the most lethal allergic disorder, which can result in immediate death. It usually occurs in community settings as the person can encounter the trigger anytime. The clinical criteria for the diagnosis of Anaphylaxis involve fulfilment of either of the three conditions shown below.
Criteria |
Accompanying conditions |
| Acute onset of illness involving skin or mucosal tissue or both. | A respiratory compromise such as dyspnea, stride, hypoxemia. |
| Reduced BP or other symptoms of end-organ dysfunction such as syncope, incontinence. | |
| Two or more of the accompanying conditions after exposure to an allergen. | Involvement of skin mucosal tissue such as hives, swollen lips-tongue-vulva. |
| A respiratory compromise such as dyspnea, wheeze, bronchospasm. | |
| Reduced BP or other symptoms such as hypotonia, syncope. | |
| Persistent gastrointestinal symptoms. | |
| Reduced BP after exposure to an allergen. | Low systolic BP. |
| Systolic BP of less than 90mmHg. |
Table 1: Clinical criteria for anaphylaxis (Sampson et al., 2006)
Different types of allergens trigger the clinical conditions shown above. Consequently, they interact with the mast cells or basophils, resulting in the release of different mediator molecules. The different allergens and the mediators released by the immune cells are shown below. Amongst different allergic reactions, the immunologic allergens are usually responsible for anaphylaxis in humans.

Epinephrine administration to treat Anaphylaxis
To counter Anaphylaxis, Epinephrine administration is the most preferred course of treatment. It acts on adrenergic receptors and counters the biological changes due to the action of mediators such as histamine. Acute Anaphylaxis demands immediate intervention, and epinephrine forms the first line of treatment. It could be administered via subcutaneous and intramuscular routes, inhalation or intravenous route (McLean-Tooke, Bethune, Fay, & Spickett, 2003). Post-administration, epinephrine acts upon different adrenergic receptors and brings about the below shown biological changes, therefore bringing relief from the clinical symptoms.

Cause of Allergic Rhinitis
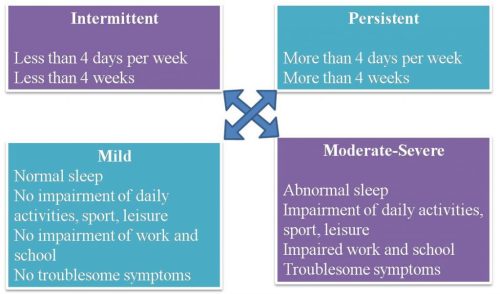
Allergic Rhinitis results from a hypersensitive response to IgE antibodies. It has four major symptoms of watery rhinorrhea, nasal obstruction, nasal itching, and sneezing. The allergic reaction results due to the release of Cytokines from the binding of antigen-specific IgE on the surface of mast cells and basophils. These resulting symptoms are classified into 4 types as shown below:
Treating Allergic Rhinitis
Accordingly, the administration of relevant treatment depends upon the level of severity of the allergy. Approach to facilitate administration of suitable treatment involves the use of the Step therapy algorithm. It is a pharmacologic treatment algorithm as shown below:

The algorithm derives its origin from evidence-based treatment guidelines and aims to provide optimal treatment for the concerned individual. The various pharmacological treatments can involve either monotherapy or combination therapy. Below shown are the different avenues for Rhinitis therapy using a single agent.
Pharmacotherapeutic agent |
Features |
| Intranasal Steroids |
|
| Oral antihistamines |
|
| Intranasal antihistamines |
|
| Leukotriene modifiers (LTRAs) |
|
| Decongestants |
|
| Anticholinergic agents |
|
| Mast cell Stabilizers |
|
Table 2: Single-agent pharmacotherapy (Meltzer, 2013)
The table below shows the different combination therapies for treating Rhinitis. In addition to these therapies, the complementary therapies and alternative medicinal treatments can also help relieve treatments of Rhinitis allergy. These include using acupuncture, herbal medicines, homoeopathy, and other physical techniques (Yonekura et al., 2016).
Pharmacotherapeutic agent |
Features |
| INS + Intranasal Antihistamines |
|
| INS + Intranasal Decongestants |
|
| Oral antihistamine + LTRA |
|
Table 3: Combination pharmacotherapy (Meltzer, 2013)
Allergic Asthma is the most prevalent allergic disease
Allergic Asthma is an aspect of Asthma, the most prevalent affecting 330 million people worldwide. The disease continues to expand as a burden on public health services on a global level. It is thought to be a complex disorder which is a result of multiple interactions occurring between environment and genetic elements. The immunological chain of response involves the stimulation of TH2 cells which produces IgE and cytokines. The repetitive exposure to allergen results in activation of mast cells, which ultimately release mediators. These mediators cause inflammation of airways (Mukherjee & Zhang, 2011). Shown below are some of the common Asthmatic allergens and their sources.
Agent |
Allergen |
| House dust mites | Der p 1, Der f 1 |
| Furry pets | Fel d 1, Can f 1 |
| Cockroaches | Tiny protein particles |
| Pests | Mus m 1, Rat 1 |
| Molds | Spores |
| Flowers | Pollens |
Table 4: Asthmatic allergens (Cipriani, Calamelli, & Ricci, 2017)
Treating allergic Asthma
The allergic form of Asthma exhibits multiple clinical and immunological phenotypes, hence a number of different treatment therapies are applicable. One such approach involves biologically targeted therapies, acting on IgE, Interleukin-4, Il-4R, Il- 13, Il-5, anti-tumor necrosis factor, and CRTh2 targets. Omalizumab, the only FDA approved biologic, acts upon IgE target, binding to the Cε3 domain of free heavy chain. It is highly effective in interrupting the allergic cascade as it blocks free IgE receptors and downregulates FcεRI receptors. The results from human studies have shown it to decrease free IgE serum level up to 99%. It also suppresses new IgE production and decreases inflammation of airways(Bice, Leechawengwongs, & Montanaro, 2014).

Another approach for treating allergic Asthma is the application of specific allergen immunotherapy (SIT). SIT aims at treating the underlying cause of allergic Asthma, rather than providing symptomatic relief. It involves repetitive administration of allergens to patients in increasing dosages. The research around the mechanism of action of the same is still going on. The therapeutic success involves a shift of T helper cells from type 2 to type 1 and production of T regulatory cells. The T regulatory cells are known to produce anti-inflammatory cytokines(Moote & Kim, 2011).

However, the degree of efficacy of SIT is still controversial.The review by Tabar (2017) on studies reporting the SIT treatment in asthma reports the administration of suboptimal treatment. Also, several patients did not report optimal asthma control.
Availability of treatment options
The treatment options for Anaphylaxis, Rhinitis, and Asthma aim towards providing symptomatic relief only and not treat the underlying causes. Anaphylaxis currently benefits from epinephrine only, where special care has to be given with respect to dosage. Although a number of relevant treatment approaches are available for Rhinitis, all of these focus on providing relief from symptoms only. Treatment options for allergic Asthma are surprisingly very limited. The sensitive nature of this disorder and its association with a prevalent disease demands new options for management and treatment.
References
- Baiardini, I., Braido, F., Brandi, S., & Canonica, G. . (2006). Allergic diseases and their impact on quality of life. Annals of Allergy, Asthma & Immunology, 97(4), 419–429.
- Bice, J. B., Leechawengwongs, E., & Montanaro, A. (2014). Biologic targeted therapy in allergic asthma. Annals of Allergy, Asthma & Immunology, 112(2), 108–115.
- Cipriani, F., Calamelli, E., & Ricci, G. (2017). Allergen avoidance in allergic asthma. Frontiers in Pediatrics, 5, 1–10.
- Larsen, J. N., Broge, L., & Jacobi, H. (2016). Allergy immunotherapy: the future of allergy treatment. Drug Discovery Today, 21(1), 26–37.
- McLean-Tooke, A. P., Bethune, C. A., Fay, A. C., & Spickett, G. . (2003). Adrenaline in the treatment of anaphylaxis: what is the evidence? BMJ: British Medical Journal, 327(7427), 1332.
- Meltzer, E. O. (2013). Pharmacotherapeutic strategies for allergic rhinitis: Matching treatment to symptoms, disease progression, and associated conditions. Allergy and Asthma Proceedings, 34(4), 301–311.
- Moote, W., & Kim, H. (2011). Allergen-specific immunotherapy. Allergy, Asthma & Clinical Immunology, 7(1).
- Mukherjee, A. B., & Zhang, Z. (2011). Allergic asthma: influence of genetic and environmental factors. Journal of Biological Chemistry, 286(38), 32883–32889.
- Pelaia, G., Gallelli, L., Renda, T., Romeo, P., Busceti, M. T., Grembiale, R. D., … Vatrella, A. (2011). Update on optimal use of omalizumab in management of asthma. Journal of Asthma and Allergy, 4, 49.
- Sampson, H. A., Muñoz-Furlong, A., Campbell, R. L., Adkinson, N. F., Bock, S. A., Branum, A., Brown, S. G., … Gidudu, J. (2006). Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Annals of Emergency Medicine, 47(4), 373–380.
- Tabar, A. I. (2017). Specific allergen immunotherapy for the treatment of allergic asthma: a review of current evidence. J Investig Allergol Clin Immunol, 27, 1–35.
- Yonekura, S., Okamoto, Y., Sakurai, D., Sakurai, T., Iinuma, T., Yamamoto, H., … Okubo, K. (2016). Complementary and alternative medicine for allergic rhinitis. Allergology International, 1–7.
Discuss